New Jersey
Our mission is to save lives by meeting the most critical needs of our communities and investing in breakthrough research to prevent and cure breast cancer.
New Jersey
Our mission is to save lives by meeting the most critical needs of our communities and investing in breakthrough research to prevent and cure breast cancer.
Need Help?
Call our breast care helpline to assist with finding local screening and diagnostic facilities or clinical research trials, requesting financial assistance, or other questions or care needs.
Get Involved
Help us reach our vision of a world without breast cancer by getting involved in our local community.

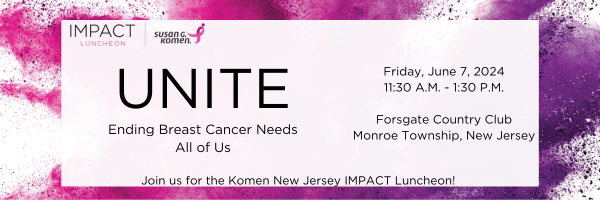
25th Annual Golf for the Cure
Registration is open for the 25th annual Komen New Jersey Golf for the Cure. Join us Oct. 14 at Metedeconk National Golf Club for breakfast and a shotgun start, with networking, cocktails and dinner following a great day of golf.
Get Involved
Make a Difference by Volunteering
create a world without breast cancer. We value all our volunteers who assist in Komen events, delivering our mission, sharing our advocacy, and more. Join us at one of our upcoming events!
QUESTIONS? CONTACT US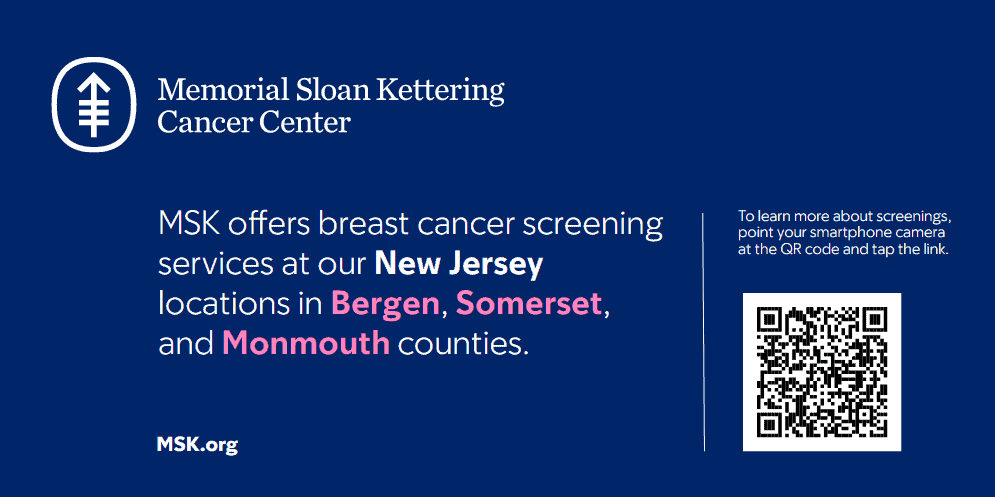
Become a Worship in Pink Ambassador for your congregation.
Sponsored locally in New Jersey by Memorial Sloan Kettering Cancer Center, ambassadors are trained to coordinate or lead activities to promote the importance of taking control of your breast health and accessing resources and support services from Komen’s Patient Care Center. Honor, celebrate, and empower the lives of those impacted by breast cancer because breast cancer can be overwhelming, but there is strength in faith.
Sign Up TodayLocal Events
Join the fight to end breast cancer by attending an event in New Jersey!
Questions? Contact Us

ShareForCures
Your breast cancer information is as unique as you are. When combined with thousands of other ShareForCures members, you provide scientists with a more diverse set of data to make new discoveries, faster.
Latest News & Information
Nikki’s Story: I’m Not Going to Let Cancer Steal My Sparkle
Nikki Anderson’s cancer journey began with a uterine cancer diagnosis in her 30s, which was followed by a breast cancer diagnosis six years later. She celebrates her journey by fundraising for the Komen 3-Day with Team Sparkle, inspired by her own adage: “I’m not going to let cancer steal my sparkle.”
The post Nikki’s Story: I’m Not Going to Let Cancer Steal My Sparkle appeared first on Susan G. Komen®.
Susan G. Komen® Peoria MORE THAN PINK Walk Raises Funds for Breast Cancer Patient Care Services in Illinois
Susan G. Komen®, the world’s leading breast cancer organization, will hold the Susan G. Komen Peoria MORE THAN PINK Walk on Saturday, May 11, 2024, at Metro Centre. This signature event enables Komen to raise critical funds that provide direct support to breast cancer patients, fund groundbreaking research, empower health equity initiatives nationwide, and advocate […]
The post Susan G. Komen® Peoria MORE THAN PINK Walk Raises Funds for Breast Cancer Patient Care Services in Illinois appeared first on Susan G. Komen®.
New Jersey
Contact Us
Susan G. Komen New Jersey

State Executive Director, New Jersey: Chelsea Beecher
Email: cbeecher@komen.org
Phone: 973-536-1251